Periodontics deals with the prevention and treatment of all diseases affecting the apparatus that supports the teeth, the periodontium.
The periodontium is the set of anatomical structures consisting of the gingiva, alveolar bone (the bone which contains the tooth), cementum and periodontal ligaments (the connective tissue that connects the tooth to the alveolar bone). The integrity of the periodontium is essential to the maintenance of oral health.
What is “Periodontitis”?
Periodontitis is inflammation of the periodontium and causes the attachment of the tooth to be lost. Today, we know that only a few bacterial species are responsible for periodontitis. These bacterial species are exogenous, or are transmitted to the host through direct contamination (kissing, sharing the same toothbrush, cutlery, etc.). Only in a few cases, however, can these bacteria lead to periodontal disease, or rather inflammation of the periodontium.
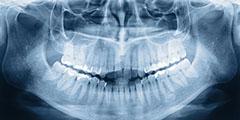
How can bone loss be verified?
The periodontal bacteria, which is responsible for periodontitis, is unable to bind to the tooth surface. To reproduce It needs what is clinically referred to as biofilm (plaque bacteria and organic residues); or rather it ‘hides’ in the plaque bacteria to protect itself from agents that attack it in the oral cavity (saliva, secretory IgA). Thus, by means of their ability to inhibit the leukotoxin through the host’s defence mechanisms, they penetrate into the gingival sulcus and destroy the connective attachment of the tooth, leading to reabsorption of the alveolar bone.
Is it possible to have a family history of periodontitis?
Yes. Many people have periodontal bacteria in the oral cavity, but show no clinical manifestation of it. This is because they simply do not have a family history of periodontitis.
What are the clinical manifestations of periodontitis?
Periodontitis can be divided into two categories:
- Chronic
- Aggressive (localised to one tooth or generalised, affecting multiple teeth)
The first type is the most common and the easiest to treat. It occurs in adults and, if diagnosed in time, it can be cured without any evident clinical manifestation. Aggressive cases, however, are usually unexpected; patients are young, with little plaque, generally healthy. In the latter case, the pathogenic hypothesis is a local - a non-systematic - defect of phagocytosis and chemotaxis of the polymorphonuclear the host’s defence cells.
There are many clinical signs of periodontitis and they vary depending on the stage and aggressiveness of the disease. To simplify, we can say that initially there is swelling in the gingiva and the interdental papillae and they may bleed. There is also a hypersensitivity to thermal stimuli and the feeling of ‘bad breath’. In more advanced cases, it may lead to significant dental mobility with the typical ‘flaring’ effect of the teeth and subsequent loss of the vertical dimensions of the mouth. Finally, it results in the loss of teeth.
What can be done to prevent periodontal disease?
Prevention requires regular visits to a professional hygienist.
During the cleaning visit, the patient should be motivated and given information about the possible risk arising from his/her habits and lifestyle choices (smoking) and shown, if necessary, the proper brushing technique.
Hygiene visits should include ultrasonic tools, hand tools (curette), prophylaxis pastes and rotating brushes to polish the surfaces of the tooth as much as possible. Tools that employ jet air are also used with polishing powders for dental cleaning. Visits should be made, on average, every four to six months. There is no valid protocol for all patients; prophylaxis should be tailored to each patient.
Something that has proved effective both as prevention and treatment is 0.2% chlorhexidine in the form of gel, spray or mouthwash that the patient should use for a time period that varies depending on the clinical indications.
If there has already been bone loss, can the bone be regenerated?
This is possible in many cases. It is necessary to first assess the type of bone loss.
Depending on the morphology of the bone defect, there are different surgical techniques that can be used.
When there is “horizontal” bone loss, or rather even bone resorption where the height of the bone in relation to the teeth is uniformly decreased, it is assumed that it does not have regenerative potential; it is not possible to regenerate lost bone. The disease is blocked by removing the infected connective tissue by polishing down the root cementum “softened” by plaque, applying a substance that can detoxify the root and, where possible, regularise the bone profile according to its physiological scalloping.
When there is “vertical” bone loss, presented as a peak bone that is higher than the bottom of the defect, however, there is the possibility to regenerate bone growth. In this situation, biomaterials (the same ones used in guided bone regeneration for implants) and amelogenin proteins in a gel form, including blood clot cells that differentiate the cell lines that are responsible for regenerated the periodontium, are used.